Breakthrough Cancer Treatment: How A New Therapy Is Melting Brain Tumors
Imagine a world where brain tumors, once considered untreatable, could be dissolved with a revolutionary new therapy. Recent advancements in medical science have brought this vision closer to reality with a groundbreaking treatment that has shown remarkable success in shrinking and even eradicating brain tumors. This innovative therapy, which leverages cutting-edge technology and scientific understanding, is already transforming the lives of countless patients. It represents a beacon of hope for those who have long battled one of the most aggressive forms of cancer. With promising results emerging from clinical trials, this new cancer treatment melts brain tumor cells in ways never seen before, offering a glimpse into a future where cancer may no longer be a death sentence.
Brain tumors have long been a formidable challenge in the medical world due to their complex nature and the delicate environment in which they reside. Traditional treatments such as surgery, radiation, and chemotherapy, while effective in some cases, often come with severe side effects and limited success rates, especially for aggressive forms like glioblastoma. However, the advent of this new treatment marks a paradigm shift in oncology. By targeting tumor cells at their core and leveraging the body’s natural defenses, this therapy has demonstrated unprecedented efficacy. Scientists and doctors are hailing it as a game-changer, not only for its ability to shrink tumors but also for its potential to minimize damage to surrounding healthy tissue.
What sets this treatment apart is its innovative approach, which combines precision medicine with advanced biotechnology. Unlike conventional therapies, which often attack both healthy and cancerous cells indiscriminately, this new method zeroes in on tumor-specific markers, ensuring that only malignant cells are targeted. Early results have been nothing short of miraculous, with some patients experiencing complete remission. As researchers continue to refine the treatment, the medical community is buzzing with excitement over its potential to revolutionize cancer care. This article delves into the science behind the therapy, its implications for patients, and what the future holds for this groundbreaking advancement in oncology.
Read also:Reba Theme Song The Iconic Melody Behind The Hit Tv Series
Table of Contents
- What Makes This New Cancer Treatment So Effective?
- How Does the New Therapy Target Brain Tumor Cells?
- The Science Behind the Treatment: Melting Tumors at the Molecular Level
- Is This Treatment the Future of Cancer Care?
- What Are the Potential Side Effects of the New Cancer Treatment?
- Success Stories: Patients Who Have Benefited from the New Therapy
- How Close Are We to Widespread Availability of the New Treatment?
- FAQs About the New Cancer Treatment Melting Brain Tumors
What Makes This New Cancer Treatment So Effective?
One of the most remarkable aspects of this new cancer treatment is its ability to specifically target brain tumor cells while sparing healthy tissue. Unlike traditional therapies that rely on broad-spectrum approaches, this treatment uses advanced precision medicine techniques to identify and attack tumor-specific markers. By doing so, it minimizes collateral damage to surrounding brain structures, which is a common issue with conventional treatments like radiation and chemotherapy. This level of precision is achieved through cutting-edge imaging technologies and molecular diagnostics, which allow doctors to map the tumor's genetic makeup and develop personalized treatment plans.
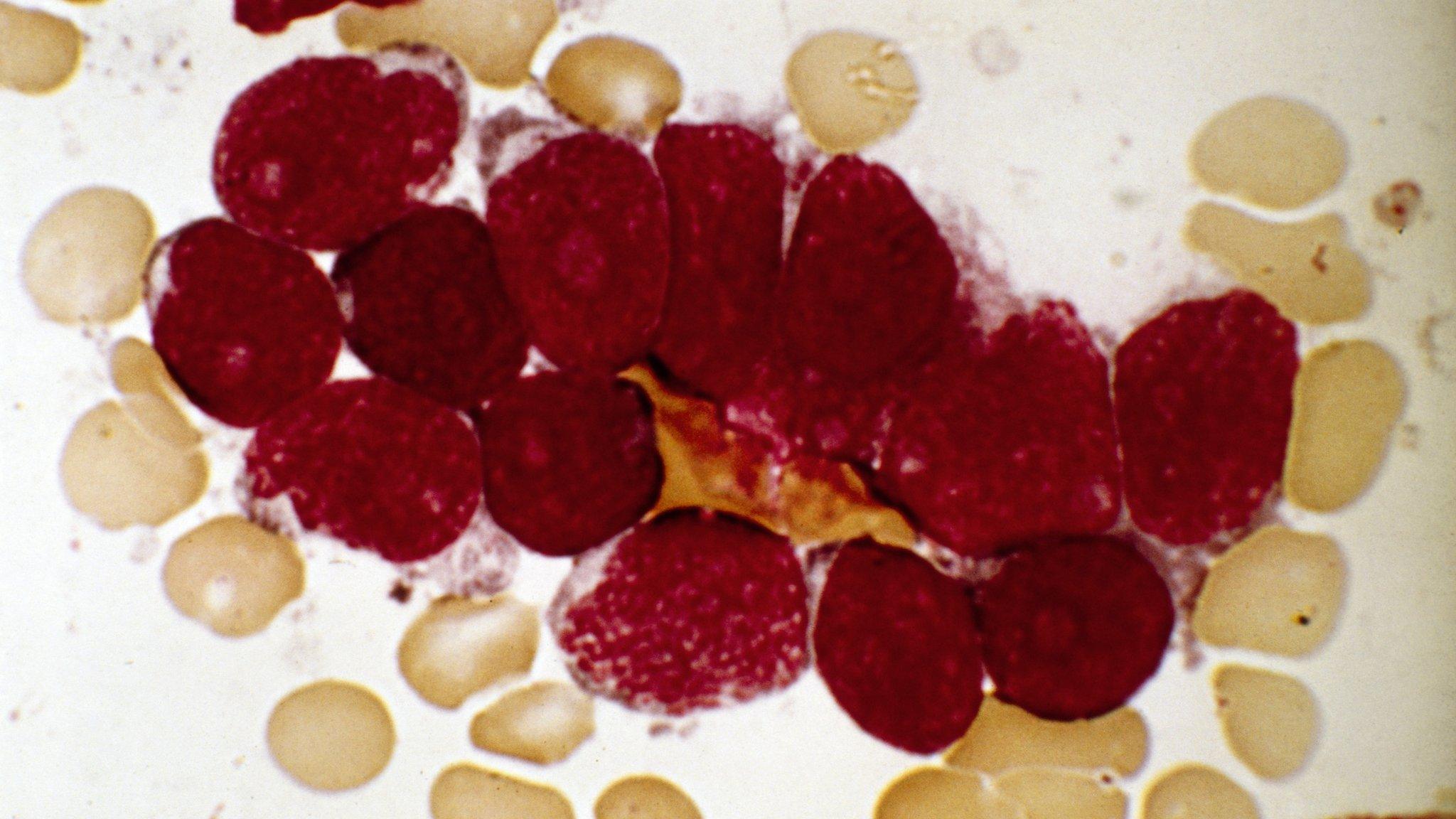
Another key factor contributing to the treatment’s effectiveness is its multi-faceted approach. The therapy combines several innovative techniques, including immunotherapy, targeted drug delivery, and thermal ablation. Immunotherapy, for example, harnesses the body’s immune system to recognize and destroy cancer cells, while targeted drug delivery ensures that medications are released directly into the tumor site. Thermal ablation, on the other hand, uses heat to "melt" tumor cells at the molecular level, effectively shrinking or eliminating them. This synergistic combination not only enhances the treatment's efficacy but also reduces the likelihood of tumor recurrence.
Furthermore, the treatment’s adaptability sets it apart from existing options. It can be tailored to suit the unique characteristics of each patient’s tumor, making it highly versatile. For instance, patients with aggressive glioblastomas may require a more intensive regimen, while those with slower-growing tumors might benefit from a less invasive approach. This flexibility ensures that the therapy can be optimized for individual needs, improving outcomes across the board. As researchers continue to refine these techniques, the treatment’s potential to revolutionize cancer care becomes increasingly evident.
How Does the New Therapy Target Brain Tumor Cells?
Understanding how this new cancer treatment melts brain tumor cells requires a closer look at its innovative mechanisms. At the heart of the therapy is its ability to exploit the unique vulnerabilities of cancer cells. Unlike healthy cells, tumor cells often exhibit specific genetic mutations or protein markers that make them stand out. These markers serve as targets for the treatment, allowing it to home in on malignant cells with remarkable accuracy. For example, the therapy uses specialized nanoparticles that are engineered to bind to these markers, delivering drugs directly to the tumor site while bypassing healthy tissue.
Another critical component of the treatment is its use of thermal ablation, a process that involves heating tumor cells to temperatures high enough to destroy them. This is achieved through focused ultrasound or laser technology, which generates localized heat within the tumor. The heat disrupts the structural integrity of cancer cells, causing them to break down and dissolve. Importantly, this process is carefully controlled to ensure that surrounding healthy tissue remains unharmed. The precision of this technique has been a game-changer, particularly for tumors located in sensitive areas of the brain where traditional surgery or radiation would pose significant risks.
In addition to these methods, the treatment leverages the power of the immune system through immunotherapy. By introducing immune-boosting agents or genetically modifying immune cells to recognize tumor markers, the therapy enhances the body’s natural ability to fight cancer. This dual approach—combining direct tumor targeting with immune activation—ensures that even microscopic remnants of the tumor are eliminated, reducing the risk of recurrence. Together, these strategies create a comprehensive treatment plan that addresses brain tumors from multiple angles, maximizing its effectiveness and offering new hope to patients.
Read also:Ambani Wedding And Kim Kardashian A Spectacle Of Luxury And Global Influence
The Science Behind the Treatment: Melting Tumors at the Molecular Level
The phrase "melting brain tumors" might sound like science fiction, but the science behind this new cancer treatment is rooted in cutting-edge molecular biology and biotechnology. At its core, the treatment targets the fundamental processes that allow tumor cells to grow and thrive. One of the primary mechanisms involves disrupting the tumor’s blood supply, a process known as anti-angiogenesis. Tumors rely on a network of blood vessels to deliver nutrients and oxygen, and by cutting off this supply, the treatment effectively starves the cancer cells. This is achieved using drugs that inhibit the formation of new blood vessels, leading to the gradual breakdown of the tumor.
Another fascinating aspect of the treatment is its use of molecular-targeted therapies. These therapies are designed to interfere with specific proteins or enzymes that are crucial for tumor cell survival. For instance, certain brain tumors overexpress a protein called EGFR (epidermal growth factor receptor), which promotes rapid cell division. By introducing drugs that block EGFR activity, the treatment halts tumor growth and triggers cell death. This targeted approach ensures that only cancerous cells are affected, sparing healthy tissue and minimizing side effects.
Perhaps the most groundbreaking element of the treatment is its ability to induce apoptosis, or programmed cell death, in tumor cells. Normally, healthy cells undergo apoptosis as part of their natural life cycle, but cancer cells often evade this process. The new therapy reactivates apoptosis pathways within the tumor, causing the cells to self-destruct. This is achieved through a combination of genetic engineering and small-molecule drugs that mimic natural cell-death signals. The result is a highly effective and precise method of eliminating brain tumors at the molecular level, offering a glimpse into the future of oncology.
Is This Treatment the Future of Cancer Care?
As the medical community continues to explore the potential of this new cancer treatment, many are asking whether it represents the future of cancer care. The answer, in many ways, is a resounding yes. The treatment’s ability to melt brain tumors with unprecedented precision and minimal side effects positions it as a transformative advancement in oncology. Unlike traditional therapies, which often come with debilitating consequences, this approach offers a more humane and effective alternative. By targeting tumor cells at the molecular level and leveraging the body’s immune system, it addresses some of the most significant limitations of current treatments.
Moreover, the treatment’s adaptability makes it a versatile tool in the fight against cancer. While its initial focus has been on brain tumors, the underlying principles could potentially be applied to other types of cancer as well. For example, the use of nanoparticles and immunotherapy is already being explored for cancers like breast, lung, and pancreatic tumors. This scalability suggests that the treatment could become a cornerstone of personalized medicine, where therapies are tailored to the genetic and molecular characteristics of each patient’s cancer.
However, challenges remain before this treatment can become widely available. Regulatory hurdles, high costs, and the need for specialized equipment and expertise are significant barriers to widespread adoption. Additionally, more research is needed to fully understand the long-term effects and potential risks of the therapy. Despite these challenges, the progress made so far is incredibly promising. As clinical trials continue to yield positive results, it’s clear that this treatment has the potential to redefine cancer care and offer hope to millions of patients worldwide.
What Are the Potential Side Effects of the New Cancer Treatment?
While the new cancer treatment that melts brain tumors offers groundbreaking benefits, it is essential to consider its potential side effects. Like any medical intervention, this therapy is not without risks, and understanding these is crucial for both patients and healthcare providers. One of the most commonly reported side effects is mild to moderate fatigue, which occurs as the body adjusts to the treatment. This fatigue is often temporary and can be managed with rest and proper nutrition. Additionally, some patients may experience localized discomfort or swelling at the tumor site, particularly when thermal ablation is used. This is typically a short-term issue and resolves as the body heals.
Another potential concern is the impact on the immune system, especially with the use of immunotherapy. While boosting the immune system to target cancer cells is a key component of the treatment, it can sometimes lead to an overactive immune response. This may result in symptoms such as fever, chills, or inflammation in other parts of the body. In rare cases, the immune system might mistakenly attack healthy tissues, a condition known as autoimmune toxicity. However, these risks are closely monitored during treatment, and medications are available to mitigate such reactions.
Finally, there is the possibility of mild cognitive or neurological effects, particularly in cases where the tumor is located in critical areas of the brain. These effects can include temporary memory lapses, difficulty concentrating, or changes in speech. Fortunately, these symptoms are often reversible and improve as the treatment progresses. By carefully tailoring the therapy to each patient’s needs and closely monitoring their response, healthcare providers can minimize these side effects and ensure the best possible outcomes. Overall, while the risks exist, they are outweighed by the treatment’s potential to save lives and improve quality of life for patients with brain tumors.
Success Stories: Patients Who Have Benefited from the New Therapy
One of the most compelling aspects of this new cancer treatment is the growing number of success stories from patients who have experienced life-changing results. Take, for example, Sarah Thompson, a 42-year-old teacher from Chicago, who was diagnosed with glioblastoma, one of the most aggressive forms of brain cancer. After undergoing multiple rounds of traditional treatments with little success, Sarah enrolled in a clinical trial for the new therapy. Within months, her tumor had shrunk significantly, and she reported feeling more energetic and hopeful than she had in years. Today, Sarah is in remission and has returned to her passion for teaching, crediting the treatment for giving her a second chance at life.
Another inspiring story is that of Michael Rodriguez, a 56-year-old father of three from Miami. Michael’s diagnosis came with a grim prognosis, as his tumor was located in a highly sensitive area of the brain. Traditional surgery was deemed too risky, leaving him with few options. However, after undergoing the new treatment, Michael experienced a remarkable recovery. Not only did his tumor melt away, but he also regained motor skills that had been impaired by the cancer. He now spends his time volunteering at cancer support groups, sharing his journey to inspire others facing similar challenges.
These stories are not isolated incidents. Clinical trials and early adopters of the treatment have reported consistently positive outcomes, with many patients achieving complete remission