Can Ablation Cause Menopause? Understanding The Link And Effects
Can ablation cause menopause? This question has become increasingly common among women considering endometrial ablation as a treatment for heavy menstrual bleeding. Endometrial ablation is a minimally invasive procedure designed to reduce or eliminate menstrual flow by destroying the lining of the uterus. While it offers relief to many women, concerns about its potential impact on menopause have sparked curiosity and debate. Understanding the relationship between ablation and menopause is crucial for making informed decisions about your health.
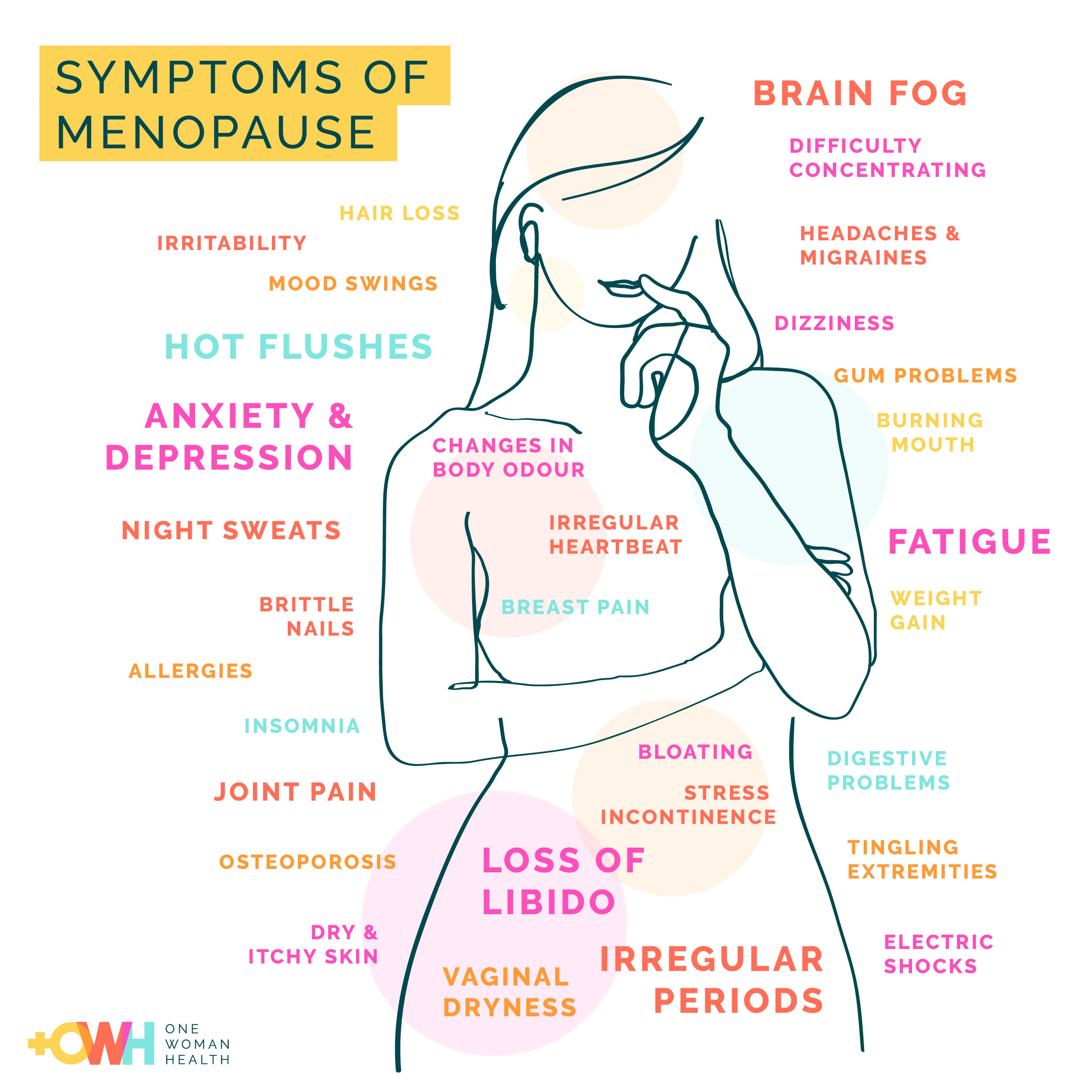
Menopause, a natural biological process, marks the end of a woman's reproductive years and is typically characterized by the cessation of menstruation. However, certain medical procedures, including ablation, can influence hormonal changes and reproductive health. While ablation is not intended to induce menopause, some women report symptoms similar to those experienced during menopause, such as hot flashes or mood swings. This overlap in symptoms often leads to confusion and raises important questions about the procedure’s long-term effects.
As we delve deeper into the topic, we'll explore the science behind ablation, its intended purpose, and whether it can indeed trigger menopause. We'll also address related concerns, such as how the procedure affects hormone levels, fertility, and overall quality of life. By the end of this article, you'll have a comprehensive understanding of whether "can ablation cause menopause" is a valid concern or a misconception that needs clarification.
Read also:What Happened To Maggie In The Walking Dead A Comprehensive Breakdown
Table of Contents
- What is Ablation and How Does It Work?
- Can Ablation Cause Menopause? Exploring the Connection
- Does Ablation Affect Hormone Levels in Women?
- What Are the Common Symptoms After Ablation?
- How Does Ablation Differ from Natural Menopause?
- What Are the Long-Term Effects of Ablation on Reproductive Health?
- Are There Alternatives to Ablation for Managing Menstrual Issues?
- Frequently Asked Questions About Ablation and Menopause
What is Ablation and How Does It Work?
Endometrial ablation is a medical procedure designed to treat heavy menstrual bleeding by removing or destroying the lining of the uterus, known as the endometrium. This lining is responsible for shedding during menstruation, and when it becomes excessively thick or problematic, it can lead to abnormally heavy periods. Ablation aims to reduce or stop menstrual flow by targeting this tissue. The procedure is minimally invasive, typically performed on an outpatient basis, and offers a less drastic alternative to hysterectomy for women seeking relief from debilitating menstrual symptoms.
There are several methods used to perform endometrial ablation, each employing different techniques to achieve the same goal. Some common approaches include thermal ablation, which uses heat to destroy the endometrial lining; cryoablation, which freezes the tissue; and radiofrequency ablation, which uses electrical currents. Regardless of the method, the goal remains consistent: to thin or eliminate the endometrial layer, thereby reducing or halting menstrual bleeding. While the procedure is highly effective for many women, it’s important to note that it is not a solution for all menstrual issues, nor is it suitable for women who wish to preserve their fertility.
Before undergoing ablation, patients typically undergo a thorough evaluation to ensure they are good candidates for the procedure. Factors such as age, medical history, and the presence of uterine abnormalities are taken into account. Additionally, hormonal treatments may be prescribed prior to the procedure to thin the endometrium, making the ablation more effective. While the procedure is generally safe, like any medical intervention, it carries risks, including infection, perforation of the uterine wall, or, in rare cases, complications that may indirectly affect hormonal balance. Understanding these nuances is crucial for anyone considering ablation as a treatment option.
Can Ablation Cause Menopause? Exploring the Connection
One of the most frequently asked questions by women considering endometrial ablation is, can ablation cause menopause? To answer this, it’s essential to differentiate between the intended effects of ablation and the natural process of menopause. Menopause occurs when the ovaries stop producing estrogen and progesterone, leading to the permanent cessation of menstruation. Ablation, on the other hand, targets only the endometrial lining and does not directly interfere with ovarian function. Therefore, the procedure is not designed to induce menopause.
However, some women report symptoms that mimic those of menopause after undergoing ablation. These may include hot flashes, night sweats, mood swings, and vaginal dryness. While these symptoms can be alarming, they are not necessarily indicative of menopause. Instead, they may result from the sudden reduction in menstrual flow or changes in the uterine environment post-procedure. It’s also worth noting that ablation may indirectly influence hormonal balance in some cases, particularly if the procedure affects the communication between the uterus and ovaries. This potential disruption can sometimes lead to temporary hormonal fluctuations, which may explain why some women experience menopause-like symptoms.
Despite these possibilities, the majority of women who undergo ablation do not experience premature menopause. Studies have shown that the ovaries continue to function normally in most cases, and women retain their ability to produce hormones until they reach the natural age of menopause. That said, individual responses to the procedure can vary, and certain factors, such as age, pre-existing hormonal imbalances, or the specific ablation technique used, may influence outcomes. For women concerned about the risk of menopause following ablation, consulting with a healthcare provider can provide clarity and reassurance. By understanding the science behind ablation and its effects on the body, women can make informed decisions about their reproductive health.
Read also:Nancy Pelosi In Hospital Today What You Need To Know
Does Ablation Affect Hormone Levels in Women?
Does ablation affect hormone levels in women? This question is central to understanding the broader implications of the procedure on a woman's reproductive health. While endometrial ablation primarily targets the uterine lining, its potential impact on hormonal balance has been a topic of interest among researchers and healthcare providers. The ovaries, which are responsible for producing estrogen and progesterone, are not directly affected by the procedure. However, the intricate relationship between the uterus and the ovaries means that changes in one can sometimes influence the other, albeit indirectly.
Research on the hormonal effects of ablation has produced mixed findings. Some studies suggest that the procedure may lead to slight hormonal fluctuations, particularly in the immediate post-operative period. For instance, the sudden reduction in menstrual flow can temporarily alter the feedback loop between the uterus and the hypothalamus-pituitary-ovarian axis, which regulates hormone production. This disruption may explain why some women experience symptoms such as hot flashes or mood swings, which are typically associated with hormonal changes. However, these effects are generally short-lived, and hormone levels tend to stabilize within a few months after the procedure.
It’s important to note that the majority of women who undergo ablation do not experience significant or long-term hormonal imbalances. Ablation does not remove or damage the ovaries, which remain fully functional in most cases. Furthermore, the procedure does not induce menopause, as it does not stop the ovaries from producing hormones. For women who do report hormonal changes, these are often attributed to other factors, such as age-related decline in ovarian function or underlying health conditions. To mitigate concerns, healthcare providers may recommend monitoring hormone levels or addressing symptoms through lifestyle adjustments or medical interventions if necessary.
What Are the Common Symptoms After Ablation?
What are the common symptoms after ablation? Women who undergo endometrial ablation often experience a range of physical and emotional changes as their bodies adjust to the procedure. While the primary goal of ablation is to reduce or eliminate heavy menstrual bleeding, the immediate aftermath can bring about symptoms that may be surprising or concerning if not properly understood. These symptoms can vary depending on the type of ablation performed, individual health factors, and how the body responds to the treatment.
Physical Symptoms
Physically, the most noticeable change after ablation is a significant reduction in menstrual flow. Many women experience lighter periods or even complete cessation of menstruation, which is often the desired outcome. However, some may notice cramping or discomfort in the days following the procedure, similar to menstrual cramps. These cramps are usually mild and subside within a week. Other common physical symptoms include:
- Vaginal discharge: A watery or bloody discharge may occur for a few weeks as the body expels the destroyed endometrial tissue.
- Fatigue: Some women report feeling unusually tired, which may be attributed to the body’s healing process or temporary hormonal shifts.
- Hot flashes: While not directly caused by ablation, some women experience hot flashes, which may be linked to temporary hormonal fluctuations.
Emotional and Psychological Symptoms
Emotionally, the post-ablation period can be a time of adjustment. Women may experience mood swings, irritability, or feelings of anxiety, particularly if they were unprepared for the changes in their menstrual cycle. These emotional symptoms are often temporary and may be exacerbated by hormonal fluctuations or the stress of undergoing a medical procedure. Additionally, some women may feel a sense of loss or grief if the procedure impacts their fertility, even if they were not planning to conceive. Counseling or support groups can be beneficial for those navigating these emotional challenges.
While most symptoms resolve within a few weeks, it’s important to monitor for any signs of complications, such as severe pain, heavy bleeding, or fever, which could indicate an infection or other issues. By understanding the range of common symptoms and their causes, women can better prepare for the recovery process and seek medical advice if needed.
How Does Ablation Differ from Natural Menopause?
Understanding the distinction between endometrial ablation and natural menopause is essential for women navigating their reproductive health options. While both involve changes to the menstrual cycle, the mechanisms, outcomes, and implications of these processes are fundamentally different. Can ablation cause menopause? is a question that often arises, but the answer lies in recognizing the unique roles of the uterus and ovaries in each scenario.
Mechanism of Action
Natural menopause is a gradual biological process that occurs when the ovaries cease producing estrogen and progesterone, leading to the permanent cessation of menstruation. This transition typically happens between the ages of 45 and 55 and is marked by symptoms such as hot flashes, night sweats, and vaginal dryness due to declining hormone levels. In contrast, endometrial ablation focuses solely on the uterine lining. The procedure destroys or thins the endometrium to reduce or stop menstrual bleeding, but it does not affect the ovaries or their hormone production. As a result, ablation does not induce menopause, though it may create symptoms that mimic those of menopause due to the sudden reduction in menstrual flow.
Impact on Fertility
Another key difference lies in the impact on fertility. Natural menopause marks the end of a woman’s reproductive years, as ovulation ceases entirely. Ablation, on the other hand, is not a sterilization procedure, although it is generally recommended for women who no longer wish to conceive. While pregnancy after ablation is rare, it is not impossible and can pose significant risks to both the mother and fetus. In contrast, menopause eliminates the possibility of pregnancy altogether, making it a definitive end to fertility.
Long-Term Effects
The long-term effects of ablation and menopause also differ significantly. Menopause is a permanent state accompanied by systemic changes, including bone density loss and increased cardiovascular risks due to hormonal decline. Ablation, however, is localized to the uterus and does not trigger systemic hormonal changes. Women who undergo ablation will still experience the natural onset of menopause when their ovaries eventually stop functioning. This distinction underscores the importance of managing expectations and understanding that ablation is a treatment for menstrual issues, not a substitute for menopause.
What Are the Long-Term Effects of Ablation on Reproductive Health?
What are the long-term effects of ablation on reproductive health? While endometrial ablation is a safe and effective procedure for managing heavy menstrual bleeding, its long-term implications on reproductive health are worth exploring. The procedure is designed to target the uterine lining, but its effects can extend beyond menstrual regulation, influencing fertility, pregnancy risks, and overall uterine health. Understanding these aspects is crucial for women who are considering ablation as a treatment option.
Impact on Fertility
Although ablation is not intended as a method of contraception, it significantly reduces the likelihood of pregnancy. The destruction of the endometrial lining makes it difficult for a fertilized